In a new Oncotarget study, researchers assessed an epigenetic and immunotherapy treatment regimen among patients with blastic mantle cell lymphoma (bMCL).
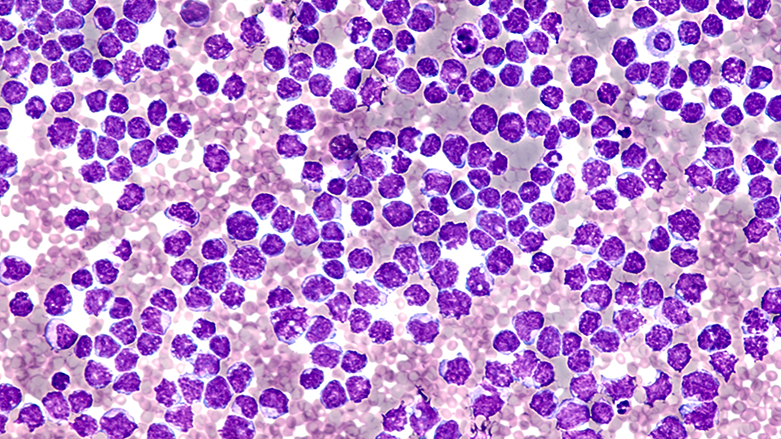
Mantle cell lymphoma (MCL) is a type of non-Hodgkin’s lymphoma (NHL) that is aggressive, difficult to treat and typically affects older adults. Recurrence and mortality rates among patients with MCL have remained high, despite recent therapeutic advances. Blastic mantle cell lymphoma (bMCL) is a rare subtype of MCL associated with a worse disease trajectory.
“Despite recent advances, MCL is incurable except with allogeneic stem cell transplant. Blastic mantle cell lymphoma (bMCL) is a rarer subtype of cMCL associated with an aggressive clinical course and poor treatment response, frequent relapse and poor outcomes.”
In previous studies, researchers reported that a combination of epigenetic and immunotherapy treatments may have synergistic activity and offer better outcomes in patients with MCL. In the current study, Francis R. LeBlanc, Zainul S. Hasanali, August Stuart, Sara Shimko, Kamal Sharma, Violetta V. Leshchenko, Samir Parekh, Haiqing Fu, Ya Zhang, Melvenia M. Martin, Mark Kester, Todd Fox, Jiangang Liao, Thomas P. Loughran, Juanita Evans, Jeffrey J. Pu, Stephen E. Spurgeon, Mirit I. Aladjem, and Elliot M. Epner from Pennsylvania State University College of Medicine, Penn State Hershey Cancer Institute, Winter Haven Hospital Cassidy Cancer Center, Icahn School of Medicine at Mount Sinai, National Cancer Institute, University of Virginia, UVA Cancer Center, University of Arizona College of Medicine, Oregon Health and Science University, and Beverly Hills Cancer Center used samples from a previous trial to perform correlative studies focused on clinical results in patients with blastic MCL. On August 16, 2022, their research paper was published in Volume 13 of Oncotarget, entitled, “Combined epigenetic and immunotherapy for blastic and classical mantle cell lymphoma.”
Epigenetic and Immunotherapy
Epigenetic therapy includes a range of drugs that can target epigenetic mechanisms, including DNA methylation and posttranslational modifications of histones. For example, vorinostat (SAHA; a histone deacetylase inhibitor) and cladribine (chemotherapy that also inhibits DNA methylation) are epigenetic agents. Rituximab, a maintenance immunotherapeutic agent, is a CD20-directed monoclonal antibody. These three treatments combined encompass a novel potential epigenetic and immunotherapy treatment regimen (SCR) for mantle cell lymphoma (MCL).
“Relapsed and [treatment] naïve MCL patients were treated with vorinostat (SAHA), cladribine and rituximab (SCR) regimen and followed for OS [overall survival], progression free survival (PFS) and with correlative basic science studies to investigate potential mechanisms of action of this epigenetic/immunotherapy combination.”
The Study
Since blastic MCL patients are rare, only 13 bMCL (four relapsed, nine previously untreated) patients treated with the SCR regimen were assessed in the prospective part of this study. All patients were male and Caucasian, and the median age at diagnosis was 62 years old. The patients were treated until they achieved remission, met the criteria for removal from the study, withdrew from the study, or passed away. Four patients were changed from rituximab to ofatumumab (a potent fully-human anti-CD20 antibody) due to rituximab intolerance (allergies, reactions) or lack of efficacy.
“Of 13 bMCL patients, all patients responded to therapy, with 12 patients meeting criteria for remission (CR, n = 6; PR, n = 6). Of those achieving CR, 5 remain in CR more than 5 years after diagnosis.”
Results
After a median of 4.8 cycles of therapy, 12 patients achieved a complete response (CR), and one patient maintained stable disease (SD). The patients reported an increased overall survival greater than 40 months, and several patients maintained durable remissions without relapse for longer than five years. These results are remarkably superior to current treatment regimens with conventional chemotherapy, which range from 14.5-24 months among bMCL patients.
“The median OS of 43.4 months and PFS of 17.3 months for MCL patients with blastic disease treated with SCR therapy is one of the most important outcomes in this study.”
Another important finding was that the G/A870 CCND1 polymorphism was a strong predictor of blastic MCL, nuclear localization of cyclinD1 and response to SCR therapy. The team identified two distinct mechanisms of resistance to SCR therapy. The researchers reported that the loss of CD20 expression and evading treatment by seeking sanctuary in the central nervous system were two major resistance mechanisms to SCR therapy.
“These data indicate that administration of epigenetic agents improves efficacy of anti-CD20 immunotherapies.”
Conclusion
Although the study sample was relatively small, the researchers’ results are promising. The SCR regimen was demonstrated to be an effective epigenetic and immunotherapy treatment for mantle cell lymphoma, with long-term remissions and improved overall survival in bMCL patients. Researchers revealed important insights into the mechanisms of action of SCR and potential resistance mechanisms. This study also highlights the potential for future research exploring the efficacy of SCR in other cancers, along with other predictive biomarkers of response.
“This approach is promising in the treatment of MCL and potentially other previously treatment refractory cancers.”
Click here to read the full research paper published by Oncotarget.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is an open-access journal that publishes primarily oncology-focused research papers in a continuous publishing format. These papers are available at no cost to readers on Oncotarget.com. Open-access journals have the power to benefit humanity from the inside out by rapidly disseminating information that may be freely shared with researchers, colleagues, family, and friends around the world.
For media inquiries, please contact media@impactjournals.com.