In a new editorial, researchers from Instituto Nacional de Cancerología discuss the obesity paradox and its potential therapeutic opportunities in the context of lung cancer.

The strong correlation between obesity and a myriad of life-limiting diseases and conditions, including type 2 diabetes, is widely recognized and acknowledged in the research community. A less defined correlation is that between obesity, diabetes and lung cancer. Whether this association is directly causal or if there are underlying contributing factors is not yet clear.
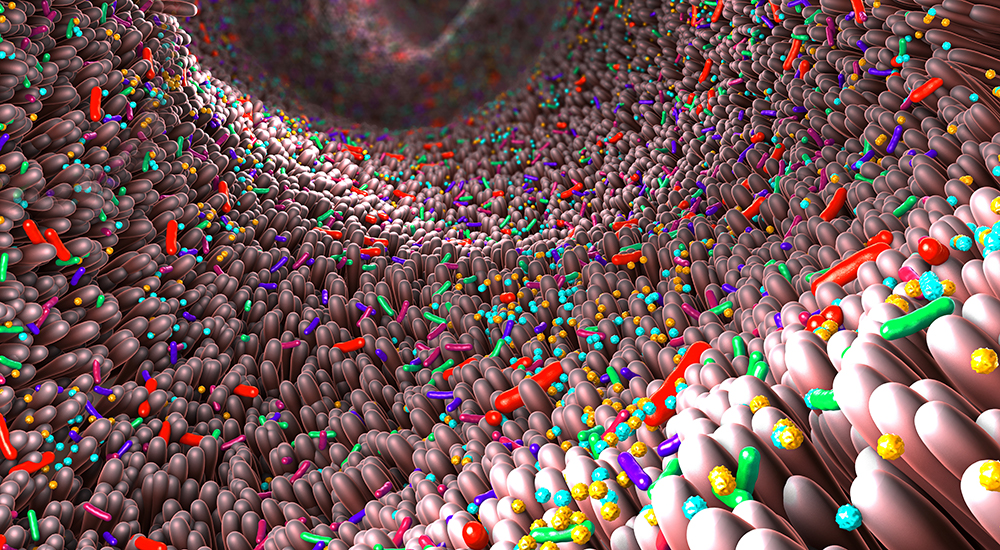
“Although obesity and type 2 diabetes mellitus (T2DM) have been associated with lung cancer (LC) development, several confounding factors, such as chronic inflammation, high insulin levels, microbiome, as well as the oncogenic potential of growth and sexual hormones, have introduced uncertainty and avoid the fully recognition of this relationship [1, 2].”
Given the existence of this association, scientists are testing therapeutic regimens that may have the potential to fight all three issues — together. Metformin, a drug commonly prescribed to treat type 2 diabetes, helps lower blood sugar levels by improving insulin sensitivity and reducing glucose production in the liver. The metabolic-modifying properties of metformin aid in treating diabetes and obesity. Metformin has also garnered attention for its potential anti-aging properties and may hold promise for treating age-related diseases, including cancer. Lately, there has been growing interest in testing metformin in combination therapies to combat cancer-promoting conditions induced by obesity.
The “Obesity Paradox”
While the link between morbidity and obesity may seem cut-and-dry, researchers have discovered a surprising trend. The “obesity paradox” suggests that, in certain instances, individuals classified as overweight or mildly obese seem to fare better or have a survival advantage compared to those with normal weight or even underweight counterparts. This paradox has been particularly observed in certain chronic illnesses, such as heart failure, chronic kidney disease, and even in the context of aging. Researchers are still striving to understand the underlying mechanisms driving this phenomenon.
In a new editorial, researchers Pedro Barrios-Bernal, Norma Hernández-Pedro, Luis Lara-Mejía, and Oscar Arrieta from Instituto Nacional de Cancerología in Mexico City, Mexico, discuss the obesity paradox and its potential therapeutic opportunities in the context of lung cancer. Their editorial paper was published in Oncotarget on July 1, 2023, and entitled, “Obesity paradox and lung cancer, metformin-based therapeutic opportunity?” They suggest that metformin may have potential therapeutic effects for both obesity and lung cancer. The researchers explore the mechanisms by which metformin may modify tumor metastatic properties and promote an antitumor immune response. They also discuss the potential implications of the obesity paradox in the context of lung cancer treatment and the potential benefits of metformin use in combination with antineoplastic therapies.
In a 2019 study, the researchers conducted a phase 2 randomized clinical trial investigating the effect of metformin combined with tyrosine kinase inhibitors (TKIs) (compared to TKIs alone) in patients with epidermal growth factor receptor (EGFR)-mutated lung adenocarcinoma. They found that the addition of metformin to standard EGFR-TKI therapy in patients with advanced lung adenocarcinoma significantly improved progression-free survival. In their 2022 study, the researchers performed a secondary analysis of the same study, now measuring the association of body mass index (BMI). This time, they reported that the survival outcome in patients with EGFR-mutated lung adenocarcinoma was greater with patients with a BMI higher than 24. The findings suggest that this treatment combination has a selective effect in obese populations and a lack of benefit in patients with a BMI less than 24, thus contributing to the obesity paradox.
“These findings suggest a strong sensitization by the addition of metformin in obese population, suggesting that biochemical and molecular differences influence the treatment response [8].”
Reflections & Future Research
In conclusion, the relationship between obesity, type 2 diabetes and lung cancer remains a subject of ongoing research. Metformin shows promise as a potential multipurpose treatment option, exhibiting properties beneficial for diabetes, obesity, aging, and cancer. The obesity paradox adds a layer of complexity to the obesity-cancer relationship, with some studies suggesting better survival rates and treatment response in overweight or mildly obese individuals treated with metformin. The researchers add that further investigation is needed to determine whether any of the proposed mechanisms of metformin have clinically meaningful activity in the treatment of obese patients with lung cancer. The ongoing research surrounding metformin and its interactions with obesity and cancer may lead to improved therapeutic strategies for these interconnected health challenges.
“Until then, we propose that pharmacodynamics, pharmacokinetics, metabolic parameters, tumor biology, biochemical and molecular modifications may be related to the ‘obesity paradox’ and must be taken into account to choose the most appropriate treatment.”
Click here to read the full editorial in Oncotarget.
—
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com. Oncotarget is indexed/archived on MEDLINE / PMC / PubMed.
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.