In this trending in vitro study, researchers assessed the efficacy of low-dose 6-mercaptopurine and 5-azacitidine to inhibit high resistance triple-negative breast cancer cells.
The Trending with Impact series highlights Oncotarget publications attracting higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news about the latest trending publications here, and at Oncotarget.com.
—
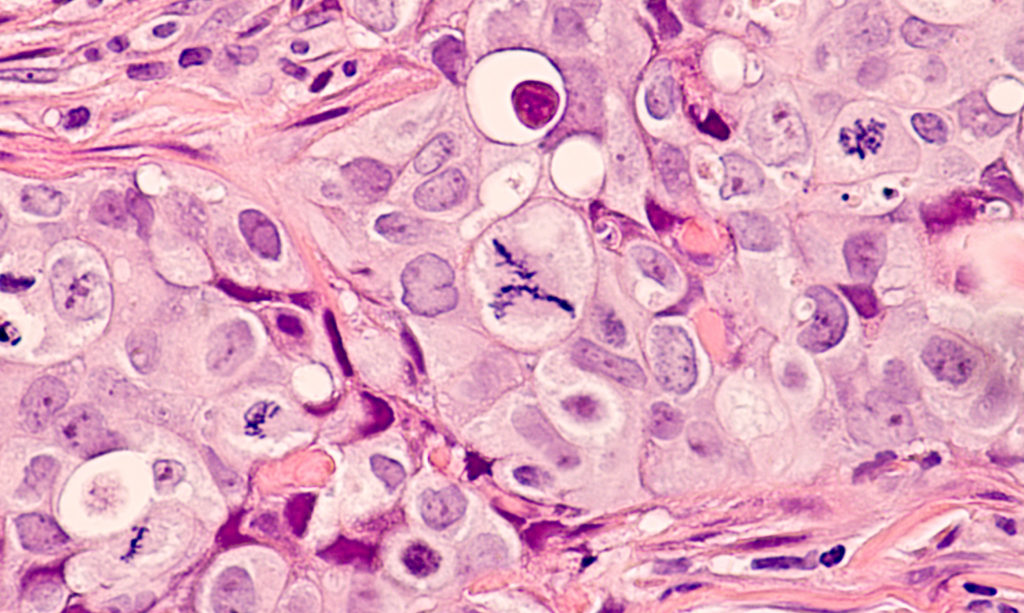
Triple-negative breast cancer (TNBC) accounts for 10-15% of all breast cancers. “Triple-negative” in this subtype of breast cancer cell refers to the lack of HER2 protein and estrogen and progesterone receptors. This means that TNBC cannot be treated with hormone inhibition and must be treated with conventional chemotherapy. In addition, many of these breast cancer cells can opportunistically switch between proliferation and quiescence—a difficult phenotype to treat. Patients diagnosed with this highly adaptable cancer frequently relapse and develop resistance to treatments.
In 2021, researchers from The University of Texas MD Anderson Cancer Center conducted a research study in hopes of developing a safe and effective therapeutic combination to treat resistant triple-negative breast cancer. Their paper, published in Oncotarget’s Volume 12, Issue 7, was entitled: “Inhibition of resistant triple-negative breast cancer cells with low-dose 6-mercaptopurine and 5-azacitidine.”
The Study
“Evidence suggests that SUM149-metabolic adaptable (MA) cells are a suitable model of resistant human triple-negative breast cancer (TNBC) cells that can survive bottlenecks in the body, including therapeutic interventions, by opportunistically switching between quiescence and cell proliferation [5, 7, 8].”
In this in vitro study, researchers cultured three highly drug-resistant and metastatic progenitor-like TNBC cell lines with opportunistic switching between quiescence and proliferation. Researchers focused on designing a safe treatment that is effective in both low- and high-risk patients. The researchers note that it was critical to their study that the regimen is proven safe to administer to patients for early use in the minimal residual disease (MRD) stage after surgery, and before clinical metastasis is detected.
“For a potential therapy to be suitable at the MRD stage, it must be safe (an important criterion prior to clinical relapse) and disrupt heterogeneous progenitor-like cancer cells that evolve into clinical metastases.”
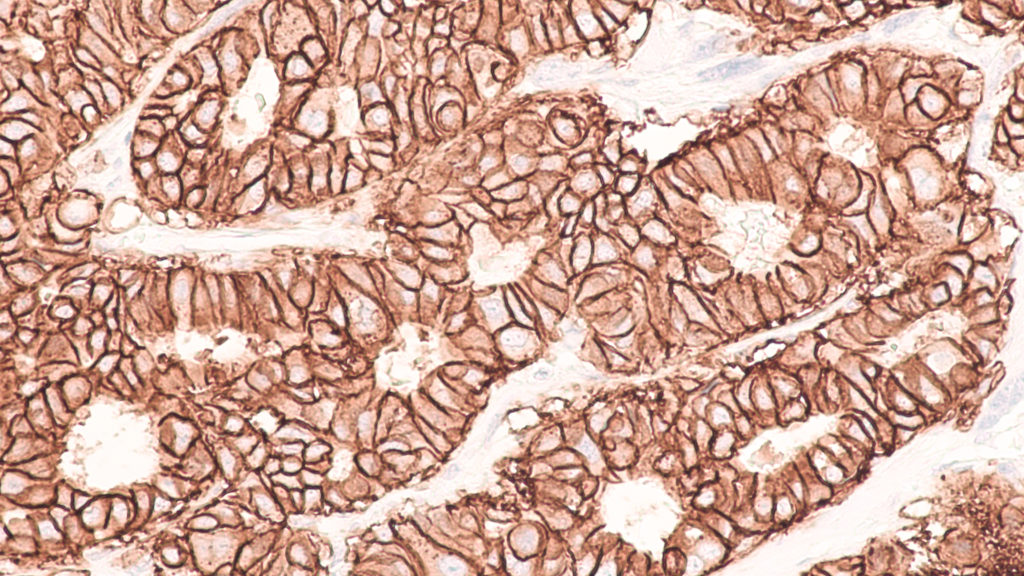
Two chemotherapy and immunosuppressive drugs (ribonucleoside analogues) were tested on the cell lines at low doses for the sake of viability in the MRD stage: 6-mercaptopurine (6-MP) and 5-azacitidine (5-AzaC). Both of these drugs have been clinically proven to be well-tolerated and to have drug-sensitizing, quiescence-stabilizing, and apoptosis-inducing effects in cancer cells.
“We chose 5-AzaC because it could complement 6-MP’s effects on the transcriptome and epigenome, and—as indicated by many Phase 1 clinical trials—5-AzaC is well tolerated [11].”
Results & Conclusion
“Our studies suggest that low-dose 6-MP, which is a purine analogue and very effective in maintaining remission in IBD [9], inhibits highly adaptable TNBC cells in our model, presumably by disrupting their transcriptome and epigenome.”
Researchers found that these low-dose therapeutics take several weeks to become effective. Despite the low dose, 6-MP (complimented by 5-AzaC) was capable of inhibiting highly adaptable TNBC cells. The researchers also point out that, based on decades of 6-MP’s use in patients with inflammatory bowel disease (IBD), this drug may be used regularly to modulate the immune system and prevent disease recurrence through its ability to inhibit chronic inflammation associated with advanced cancers.
“We suggest that low dose 6-MP and other drugs that would complement 6-MP’s action, such as 5-AzaC, could be suitable for preventing recurrence and metastasis in high-risk breast cancers. 6-MP could be taken lifelong if it is necessary for maintaining a long-term remission.”
Click here to read the full scientific study, published by Oncotarget.
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.