For the past four summers, Impact Journals has sponsored Team Open Access in the Ride for Roswell. The peloton has been captained by Sergei Kurenov, who is the Director of Surgical Simulation at Roswell Park Comprehensive Cancer Center — one of the leading cancer treatment and research centers in the nation. This year, Team Open Access was one of the many teams that participated to raise more than $5 million to help find a cure for cancer.
Prior to the 2021 Ride for Roswell (#RFR21) on August 7, we asked Sergei for his thoughts on the experience and motivation for riding.
Please tell us how you got started in the Ride for Roswell event and what pushes you to participate each year.
Kurenov: When I started working at Roswell Park Comprehensive Cancer Center, I saw how enthusiastically people supported this event and made a lot of contributions of their time in fundraising, patient care support, and cancer research. I wanted to be a part of this community.
This will be your fourth year as team captain and sixth year participating in the Ride for Roswell. What has been your most memorable year or moment since you’ve started?
Kurenov: My first year of the Ride is the most memorable. More than a few thousand riders performed the National Anthem. Then, all the riders cheered on the cancer survivors, reminding us of exactly why we participate.
During last year’s Summer of the Ride, you were a part of over 600 teams that rode to raise more than $3.6 million in the fight against cancer amid a global pandemic. Looking back, how has that specific Ride impacted your outlook on this year’s event and cancer research?
Kurenov: The pandemic has highly affected cancer research. Physicians and researchers are working very hard to minimize pandemic impact and get life back to normal for our patients.
This year, we already raised [more than] $5 million, which will be provided to the development of cancer treatments and cancer research.

Tell us a little bit about the 2021 Open Access team.
Kurenov: The 2021 Open Access team has grown again and now we have nine team members, ranging in ages from 13 to 65. Most of the members are scientists in the cancer research field.
Who is the fastest team member? The longest tenured teammate of yours? And, why do you think you make the perfect captain for this team?
Kurenov: Andrei is a great rider and I believe he is the fastest team member.
Liliya and Elena are the longest-tenured teammates for the last six years. They provide a tremendous help in the fundraising and in team organizing. They are also great photographers, making memorable images during the Ride. Each year, they create special Open Access team t-shirts which we are proud to wear during the Ride.
Who, or what, will you be focusing on as team captain this time around?
Kurenov: This year, Sofia joined the Open Access team. She is 13 years old and wants to ride 10 miles. Sofia and the rest of our team will ride together. Perhaps I will join the team or will have a barbecue for the whole team to celebrate afterwards.
How do you generally celebrate following the Ride?
Kurenov: After the Ride, all team members and many of our friends from Buffalo are planning to join a barbecue party in our backyard. Everyone is very welcome to the party.
Please give us your best pitch for people to start or continue donating to cancer research.
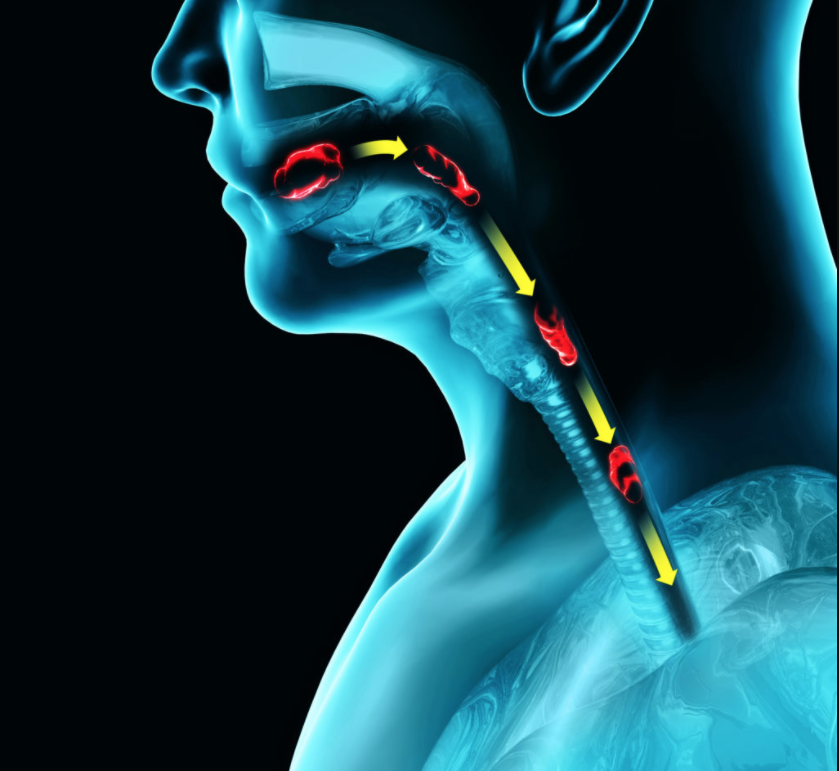
Kurenov: Earlier this year, I lost a very close friend who had fought against cancer for the last 17 years. When he was diagnosed, doctors predicted around 10 years of his survival after the initial treatment. However, thanks to the cancer research and new treatment developments in oncology, he almost doubled the doctors’ predictions. And, until this year, he lived a full life, working on cancer research, organizing scientific conferences, traveling around the world and making great photographs. His example shows that the constant cancer research and new technologies can help oncological patients. So, please continue donating to cancer research. This certainly will help to cure cancer more efficiently and save more lives.
Just like we requested of you last year, give us your best pitch for folks to join Team Open Access in 2022.
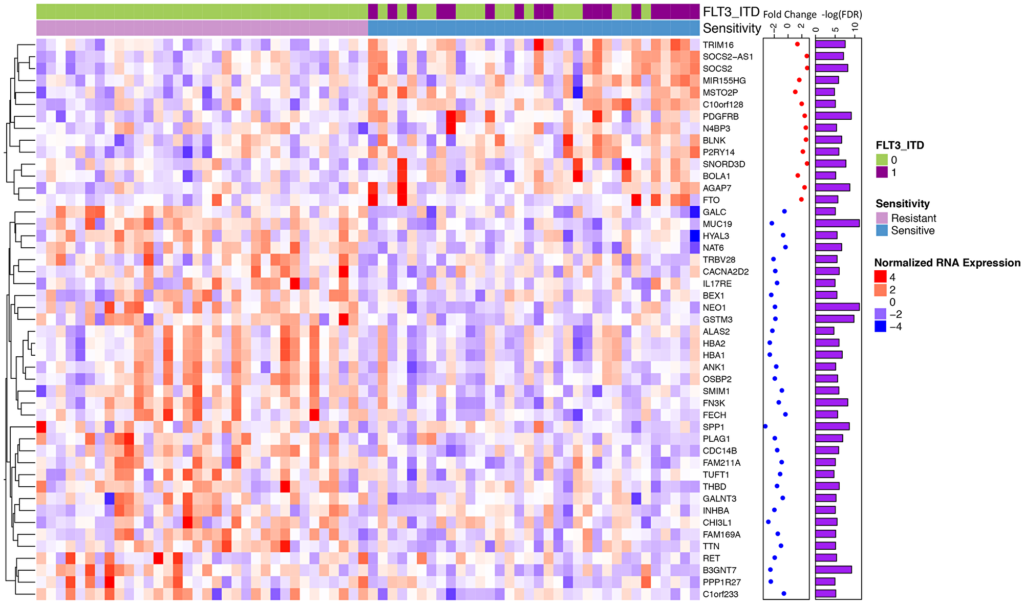
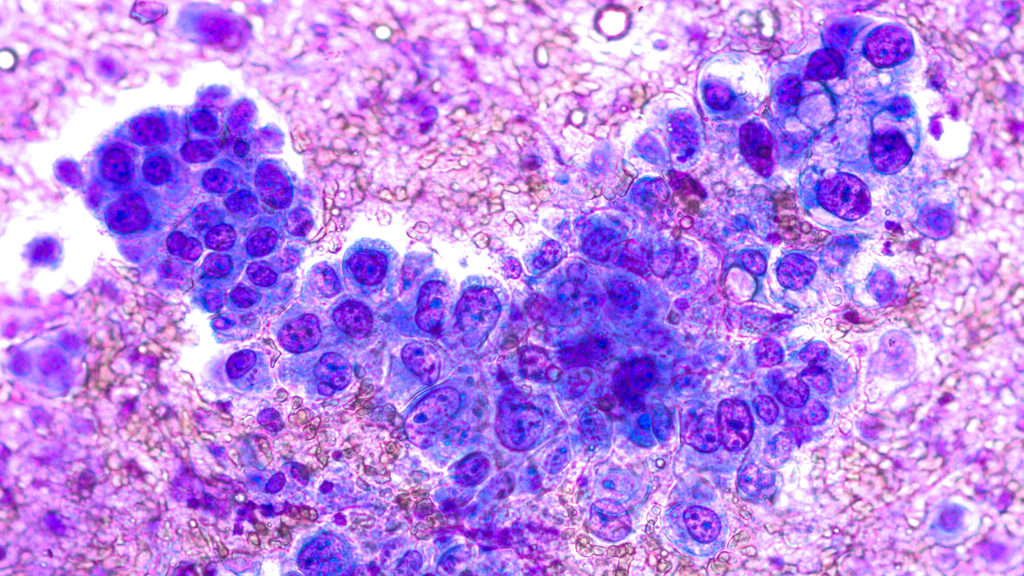
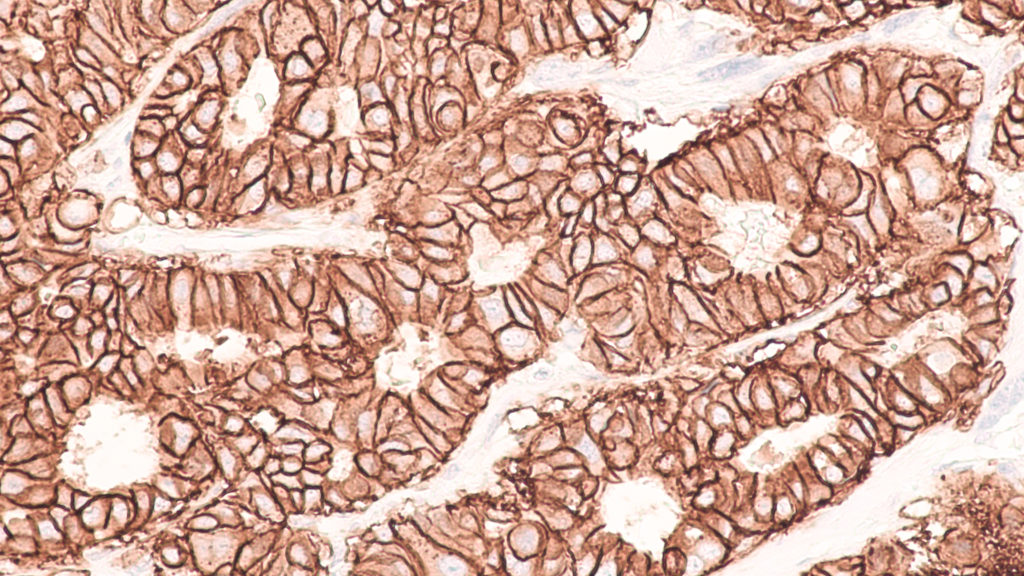
Kurenov: I am proud to announce that our team is supported again by Impact Journals – which publishes open-source, cancer-related scientific journals Oncotarget, Aging, Genes & Cancer and Oncoscience. These journals include high-impact research papers of general interest and biological significance in all fields of cancer research. As an example, I would like to mention the studies published by Impact Journals that cycling is linked to a substantial decrease in the risk of developing and dying from cancer or heart disease.
Join our team and help us reach our goal or donate to our efforts! No matter how you choose to support us, YOU are making a difference in the lives of the thousands of patients who turn to Roswell Park Comprehensive Cancer Center for hope each year.
Click here to learn more about the Ride for Roswell.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.