In this editorial, researchers delve into the immunotherapeutic challenges posed by the tumor microenvironment and liver metastasis in pancreatic cancer.
—
Pancreatic ductal adenocarcinoma (PDA), a common type of pancreatic cancer, has proven to be largely resistant to immunotherapy, a treatment that uses the body’s immune system to fight cancer. Despite numerous successful pre-clinical trials using sophisticated PDA mouse models, clinical trials have failed to show a significant improvement in survival.
In a recent editorial, researchers Brian Diskin, Sarah Schwartz and George Miller from Trinity Health of New England shed light on the complex interplay between the immune system and pancreatic cancer. Their paper was published in Oncotarget on April 24, 2023, and entitled, “The critical immune basis for differential responses to immunotherapy in primary versus metastatic pancreatic cancer.”
Tumor Microenvironment and Liver Metastasis: Challenges in Pancreatic Cancer
The authors attribute PDA immunotherapy resistance to the unique characteristics of the tumor microenvironment (TME). The TME is often hypoxic and fibrotic, making it inaccessible to immune cells. Furthermore, the immune cells that do infiltrate the TME often have tolerogenic features, meaning they are more likely to tolerate the presence of cancer cells rather than attack them.
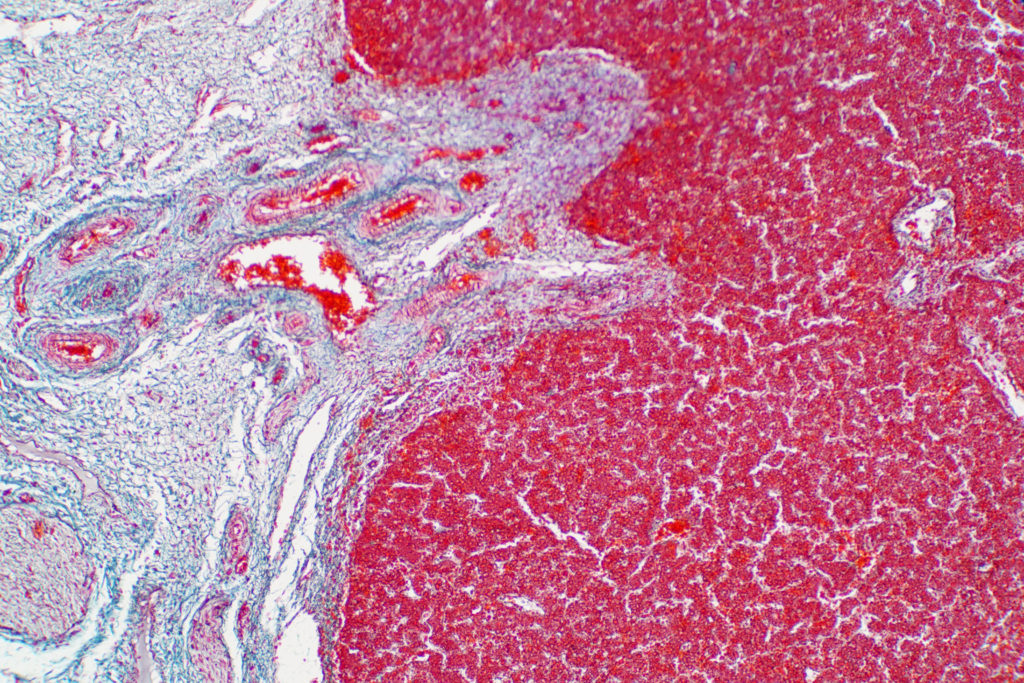
PDA most commonly metastasizes to the liver, an organ known for its immune tolerance. The liver is home to a diverse array of innate immune populations, including NK cells, Kupfer cells, NKT cells, and double negative T cells. Despite this, the liver is the most common location for metastasis from gastrointestinal cancers.
“It is an unfortunate fact that all failed clinical trials assessing immunotherapeutic efficacy were conducted in metastatic PDA, whereas basic preclinical investigations are usually performed in primary PDA using genetically engineered mouse models. We postulated that this dichotomy may explain the gap between preclinical promise and ultimate clinical failure.”
Divergent Responses to Immunotherapy: Primary vs. Metastatic
“The potentially divergent responses to immunotherapy in the respective environments of primary versus metastatic PDA within the same host has not been well-studied.”
The authors highlight the lack of research into the potentially divergent responses to immunotherapy in primary versus metastatic PDA. They argue that this gap in knowledge may explain the discrepancy between the promising results of pre-clinical trials and the disappointing outcomes of clinical trials.
In their research, they discovered that the TMEs of primary PDA and liver metastases differ significantly, and this difference plays a critical role in the site-specific response to immunotherapy. They found that liver metastases are uniquely resistant to immunotherapies, in stark contrast to the immunotherapeutic responsiveness of primary PDA.
“We discovered that the respective TMEs of primary PDA and liver metastases differ markedly and this fact plays a critical role in dictating site-specific PDA response to immunotherapy [6].”
The Role of B Cells
The researchers identified B cells as a key player in this differential response. They found that B cells constituted approximately 25% of the tumor-infiltrating lymphocytes in metastatic PDA liver deposits, compared to approximately 10% in primary PDA. They also discovered a novel population of CD24+CD44–CD40– B cells in the metastatic liver, which is recruited to the metastatic milieu by Muc1hiIL18hi tumor cells.
“[…] by targeting B cells or blocking CD200/BTLA, we demonstrated enhanced macrophage and T-cell immunogenicity, which enabled immunotherapeutic efficacy of liver metastases.”
However, the authors note that primary PDA sites lack this b-cell population. Instead, they are characterized by macrophages and effector T cells that have a higher ability to provoke an immune response. This makes their immunotherapeutic responsiveness far more robust than metastatic liver PDA.
Conclusion
This research underscores the importance of understanding the immune basis of differential responses to immunotherapy in primary versus metastatic pancreatic cancer. It highlights the need for further research into the role of the TME and immune cells like B cells in the response to immunotherapy. Such insights could pave the way for more effective treatments for this challenging disease.
“[…] our data suggest that models of primary PDA are poor surrogates for evaluating immunity or treatment response in advanced disease.”
Click here to read the full editorial paper in Oncotarget.
—
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com. Oncotarget is indexed/archived on MEDLINE / PMC / PubMed.
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.