“This case adds to the literature on bypass signaling as a mechanism of resistance to lorlatinib, providing evidence for RET activation as a novel escape mechanism […]”
What if a cancer treatment worked—until it suddenly didn’t? A new case report, “Acquired RUFY1-RET rearrangement as a mechanism of resistance to lorlatinib in a patient with CD74-ROS1 rearranged non-small cell lung cancer: A case report,” published in Oncotarget, reveals how a non-small cell lung cancer (NSCLC) patient developed drug resistance through a rare genetic alteration, allowing the cancer to evade therapy. This unexpected finding highlights the importance of advanced genetic testing and personalized cancer treatments.
Non-Small Cell Lung Cancer, Targeted Therapy and Drug Resistance
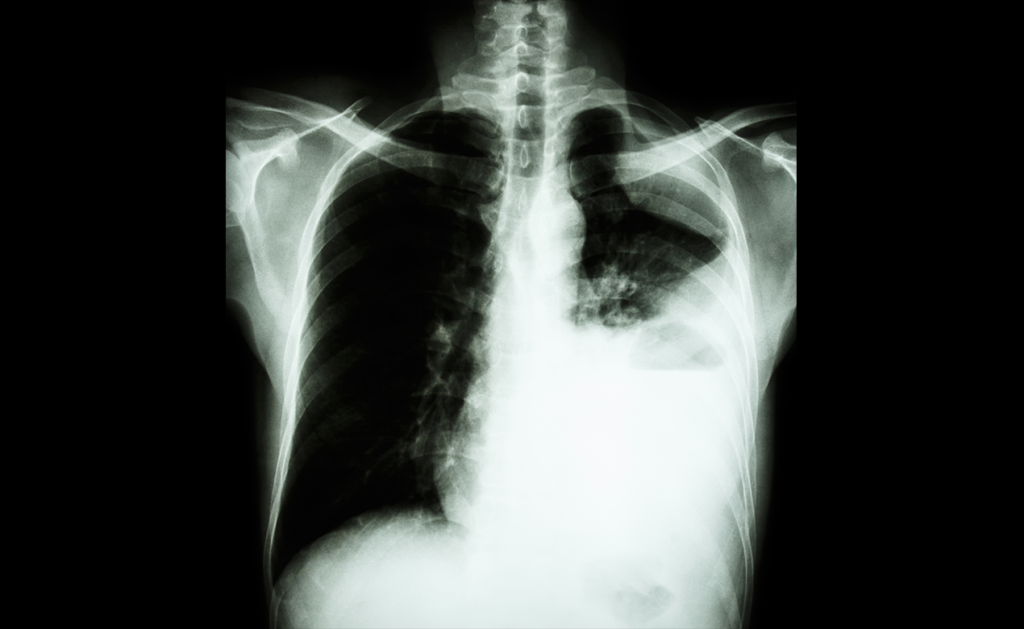
Non-Small Cell Lung Cancer is the most common type of lung cancer, accounting for nearly 85% of all cases. Some patients with NSCLC have genetic mutations, such as ROS1 gene fusions, that drive tumor growth. These patients often respond well to targeted therapies like lorlatinib, a ROS1 inhibitor that blocks cancer growth.
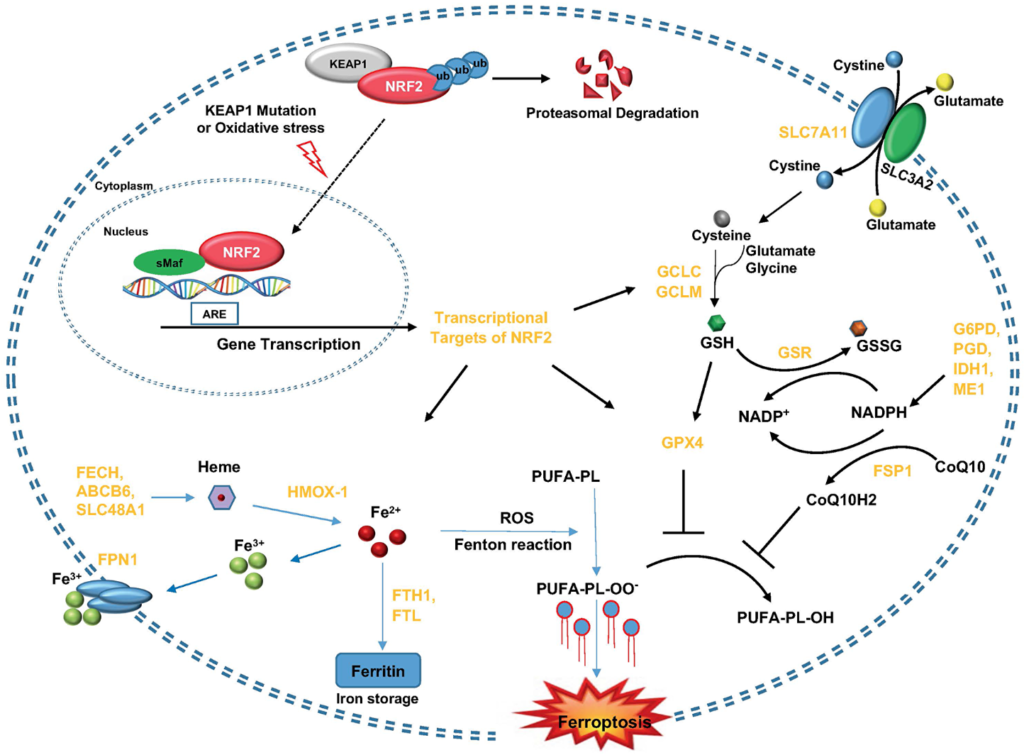
However, cancer is constantly evolving. Over time, it can develop resistance to targeted therapies, leading to treatment failure. Understanding these resistance mechanisms is crucial for precision oncology, the approach of tailoring cancer treatment based on a patient’s unique genetic profile.
The Case Report That Changed Our Understanding
Dr. Jenny L. Wu from Vanderbilt University School of Medicine and Dr. Wade T. Iams from Vanderbilt-Ingram Cancer Center describe a rare case of drug resistance in a 42-year-old man with advanced NSCLC (stage IV) carrying a ROS1 gene rearrangement. Initially, the patient responded to multiple treatments, including entrectinib and later lorlatinib, both FDA-approved ROS1 inhibitors.
After six months on lorlatinib, his cancer began progressing again. To determine why the treatment stopped working, clinicians performed RNA next-generation sequencing (NGS), a diagnostic tool used to detect genetic mutations in cancer cells.
A Hidden Genetic Mutation
The NGS revealed a previously unknown mutation: a RUFY1-RET gene fusion, which had never been linked to lorlatinib resistance before. RET fusions are commonly associated with thyroid cancer and lung adenocarcinoma, but this was the first documented case where a RET fusion emerged as a mechanism of resistance to ROS1 inhibitors.
This discovery suggests that NSCLC can activate alternative survival pathways when ROS1 inhibitors are used, making precision medicine strategies even more critical for advanced lung cancer patients.
A New Treatment Approach
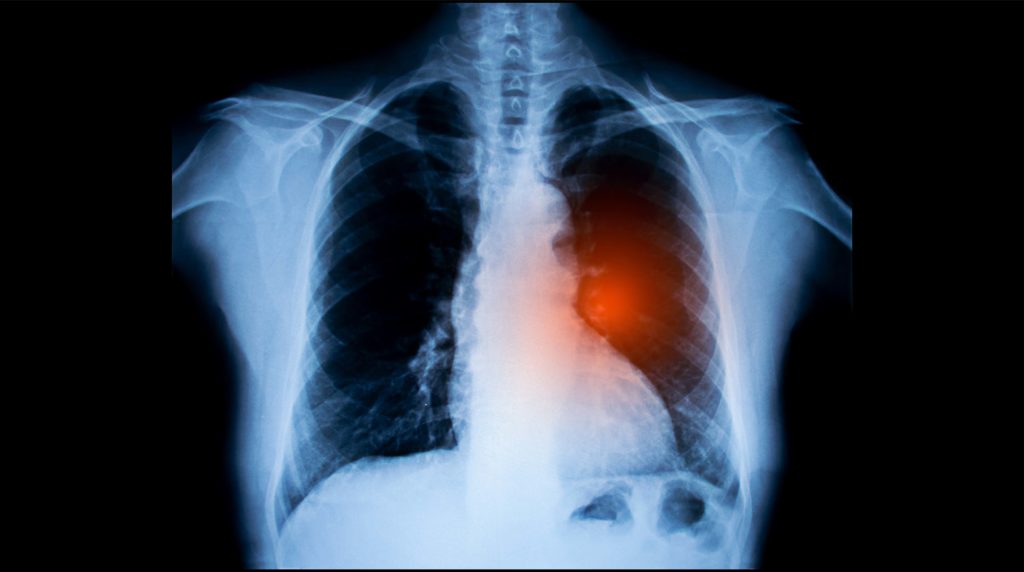
After detecting the RET fusion, clinicians adjusted the patient’s treatment plan by introducing pralsetinib, a RET inhibitor, alongside lorlatinib to target both mutations.
Initially, the combination therapy showed promise. Scans revealed tumor shrinkage, and the patient responded positively. Unfortunately, the response lasted only four months before the cancer progressed again. The patient passed away shortly thereafter, highlighting the urgent need for more durable treatment options for drug-resistant lung cancer.
The Importance of This Case
This is the first documented case of a RET fusion emerging as a resistance mechanism to lorlatinib. It challenges previous assumptions about how NSCLC adapts to targeted therapies and emphasizes the importance of RNA sequencing in detecting hidden resistance mutations.
Standard DNA testing did not detect the RET fusion; only RNA sequencing revealed it. This finding suggests that more sensitive genetic testing should be used when patients develop treatment resistance.
This case also raises new questions about therapy combinations. While the mix of lorlatinib and pralsetinib provided temporary disease control, it was not enough for long-term remission. New strategies are needed to develop more long-lasting treatment combinations for patients who develop resistance.
Future Perspectives and Conclusion
Treatment resistance remains a major challenge in lung cancer care. While targeted therapies have revolutionized treatment, they must continuously adapt to stay ahead of the disease.
Although the combination of pralsetinib and lorlatinib initially showed some effectiveness, the response did not last. In the future, scientists must investigate why some RET fusions make drugs less effective and whether finding these genetic alterations earlier could help change treatment plans before resistance fully sets in.
By uncovering new resistance mechanisms, this case highlights the importance of advanced genetic testing and contributes to the growing field of precision oncology. The more we understand how cancer adapts, the better we can develop smarter, more effective treatments and improve survival rates for lung cancer patients.
Click here to read the full case report in Oncotarget.
___
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.