In this study, researchers show that treatment of 4T1-12B mouse breast cancer cells with this nanobody inhibits V-ATPase-dependent acidification of the media and invasion of these cells in vitro.
—
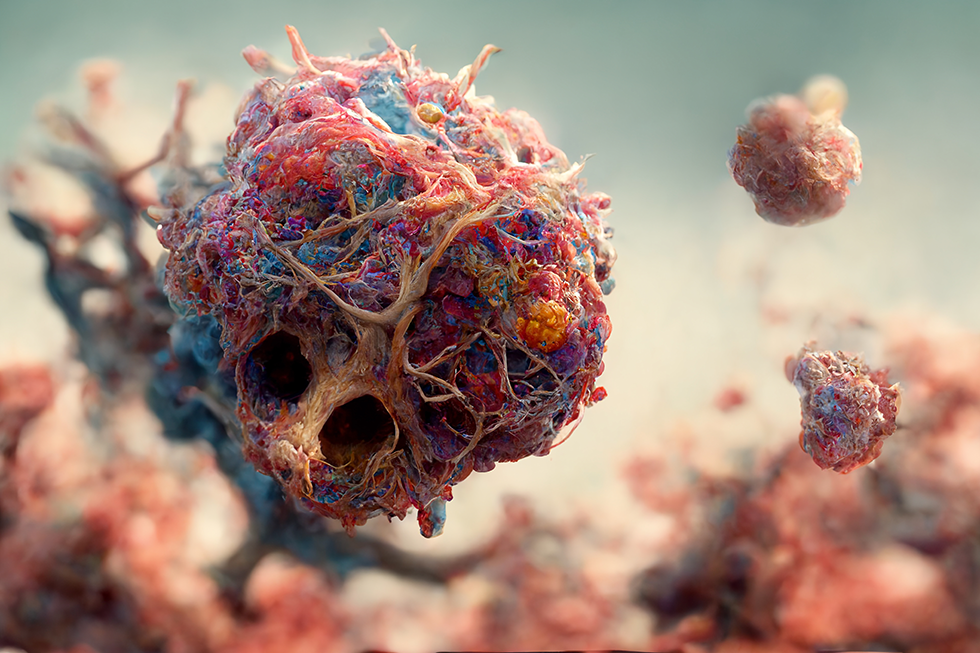
Researchers recently developed a nanobody directed against an extracellular epitope of the mouse V-ATPase c subunit. Zhen Li, Mohammed A. Alshagawi, Rebecca A. Oot, Mariam K. Alamoudi, Kevin Su, Wenhui Li, Michael P. Collins, Stephan Wilkens, and Michael Forgac from Tufts University School of Medicine; Tufts University; Dana Farber Cancer Institute, Harvard Medical School; University of Minnesota School of Medicine; Prince Sattam Bin Abdulaziz University; Korro Bio; SUNY Upstate Medical University; and Foghorn Therapeutics, suggest that plasma membrane V-ATPases represent a novel therapeutic target to limit breast cancer metastasis. The vacuolar H+-ATPase (V-ATPase) is an ATP-dependent proton pump that functions to control the pH of intracellular compartments as well as to transport protons across the plasma membrane of various cell types, including cancer cells.
On August 14, 2024, their research paper was published in Oncotarget’s Volume 15, entitled, “A nanobody against the V-ATPase c subunit inhibits metastasis of 4T1-12B breast tumor cells to lung in mice.”
The Research
Breast cancer is one of the most diagnosed cancers, accounting for almost one-third (30%) of all new diagnoses in women in 2022. At the time of diagnosis, 20–30% of patients with early-stage breast cancer will go on to develop metastatic breast cancer. 6–10% of all patients with breast cancer have stage IV disease at time of diagnosis. It has been shown that V-ATPase plays an important role in promoting the invasiveness of many cancer cell types, including breast cancer cells.
This study demonstrated that inhibiting cell surface V-ATPases can effectively block tumor cell invasion. The findings indicate that anti-V-ATPase antibodies targeting an extracellular region of the V-ATPase can suppress activity on the surface of cancer cells, as well as inhibit both in vitro invasion and in vivo metastasis in a mouse model. This represents a promising advancement toward developing a new therapy to limit breast cancer metastasis.
Results
A camelid nanobody against the N-terminus of the mouse V-ATPase c subunit was prepared using phage display. The nanobody was dimerized through disulfide bonding to create a bivalent molecule. The purified nanobody was detected using Coomassie blue staining and Western blotting. The apparent molecular weight of the dimer on SDS-PAGE was around 45 kDa, slightly faster than the predicted weight of 56.8 kDa. The nanobody was tested for its ability to inhibit V-ATPase-dependent acidification in mouse 4T1-12B cells. The nanobody treatment resulted in a similar increase in extracellular pH as treatment with concanamycin, a known V-ATPase inhibitor.
Combining both the nanobody and concanamycin did not significantly enhance the effect. The nanobody effectively inhibited V-ATPase-dependent extracellular acidification without affecting cell viability. The anti-V-ATPase nanobody was tested for its ability to inhibit in vitro invasion of 4T1-12B cells. Treatment with the nanobody significantly inhibited invasion, like its inhibition of extracellular acidification. The nanobody effectively inhibits both extracellular acidification and in vitro invasion of 4T1-12B cells with similar affinity.
The administration of the anti-V-ATPase nanobody was tested to determine its effect on tumor growth and metastasis in mice. Different amounts of the nanobody were administered to mice without any adverse effects. The effect of nanobody administration on in vivo metastasis was then tested using 4T1-12B cells implanted in the mammary fat pad. However, no significant difference in tumor volumes was observed between the control and nanobody-treated groups at the end of the study. Treatment with the anti-V-ATPase nanobody resulted in a significant reduction in lung metastasis but had no effect on tumor growth or leg metastases. No significant metastasis was observed in other organs. In contrast, treatment with the anti-GFP nanobody did not reduce lung metastases.
Discussion
The researchers’ previous results demonstrated that selective inhibition of cell surface V-ATPases using an antibody or bafilomycin showed potential in inhibiting invasion of breast cancer cells. However, the use of antibodies against the native c subunit proved challenging due to its conservation and limited exposure. To overcome this, a nanobody against a native epitope of the c subunit was developed through in vitro screening. This nanobody successfully inhibited cell surface V-ATPase activity in mouse 4T1-12B breast cancer cells and showed a correlation between inhibition of invasion and extracellular acidification. In mice, the nanobody treatment significantly reduced lung metastases, but had no effect on tumor growth or leg metastasis.
The study suggests that different mechanisms may be involved in tumor cell invasion in different tissues. The potential side effects of inhibiting cell surface V-ATPases were also discussed, highlighting the limited presence of these pumps in certain cells and the potential benefits of inhibiting osteoclast function for breast cancer metastasis to bone.
Overall, the findings support the use of inhibitory nanobodies against cell surface V-ATPases as a potential therapeutic approach to inhibit breast cancer metastasis.
“These results provide support for the use of an inhibitory antibody directed against an extracellular epitope of the V-ATPase as a potential anti-metastatic therapeutic to inhibit breast cancer metastasis.”
Click here to read the full research paper in Oncotarget.
—
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.