“[…] targeting PRDX1 should sensitize tumours to DNA-damaging agents.”
Scientists have uncovered a promising new strategy to weaken cancer cells’ natural defense mechanisms, potentially making chemotherapy more effective. In a study published in Volume 16 of Oncotarget, researchers identified the protein PRDX1 as a key player in helping tumors resist treatment. By targeting this protein, they propose a novel way to combat aggressive, treatment-resistant cancers.
Understanding Why Some Cancers Resist Treatment
Chemotherapy works by damaging the DNA of cancer cells, forcing them to self-destruct. However, many cancers develop robust repair systems that fix this damage, allowing the tumor to survive and grow. A central component of this repair machinery is a protein called ATM, which acts like a first responder in the cell, detecting DNA damage and coordinating its repair.
In ovarian cancer and other aggressive tumors, high levels of ATM have been associated with poor survival rates and resistance to chemotherapy.
The Study: How PRDX1 Protects Cancer Cells
The study, titled “PRDX1 protects ATM from arsenite-induced proteotoxicity and maintains its stability during DNA damage signaling,” was led by first author Reem Ali and corresponding author Dindial Ramotar from Hamad Bin Khalifa University in Qatar, in collaboration with researchers from the University of Nottingham in the UK.
To investigate PRDX1’s role, the team used human cell line models where they inactivated the PRDX1 gene to see how the cells would behave without it. Next, they exposed these cells to arsenite—a toxic substance that damages DNA—as well as to chemotherapy drugs and ATM inhibitors. This allowed them to observe how the absence of PRDX1 affected the cells’ ability to survive and repair damage.
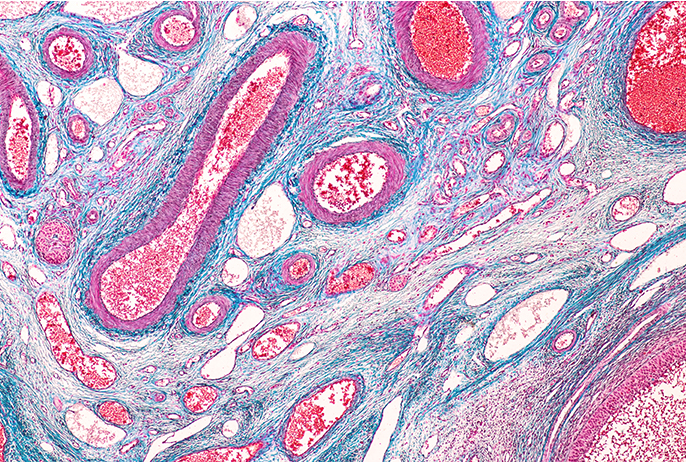
They also analyzed 183 tumor samples from ovarian cancer patients, studying the levels of PRDX1, ATM, and another DNA repair protein called MRE11, and associating these findings with patient outcomes.
The Results: PRDX1 as a Key Protector
The researchers discovered that PRDX1 physically interacts with ATM, acting as a stabilizer and protector for this critical DNA repair protein. When PRDX1 was removed from cancer cells in laboratory experiments, ATM levels decreased dramatically. Without PRDX1, the cells lost their ability to repair DNA damage and became highly sensitive to DNA-damaging agents, such as arsenite, known to harm DNA and proteins. These compromised cells were even more vulnerable when exposed to a combination of arsenite and ATM inhibitors, resulting in rapid cell death.
In tissue samples from ovarian cancer patients, tumors that had high amounts of both PRDX1 and ATM were associated with worse patient’ survival rates and were less responsive to platinum-based chemotherapy, which is a standard treatment for ovarian cancer.
Implications: A New Strategy Against Chemotherapy Resistance
This research positions PRDX1 as both a protector of cancer cells and a potential weak point. By disrupting PRDX1’s protective role, scientists believe they can sensitize resistant tumors to platinum-based chemotherapy, which is widely used for ovarian and other cancers.
The findings also raise the possibility of using PRDX1 as a biomarker to predict which tumors are more likely to respond to DNA-damaging therapies. For patients whose cancers show high PRDX1 levels, combining existing drugs with PRDX1 inhibitors, or even small doses of arsenite, might enhance treatment outcomes.
Future Perspectives and Conclusion
While these study findings are still in the experimental stage, they offer a new approach to overcoming one of cancer treatment’s greatest challenges: resistance. The next steps involve developing safe ways to block PRDX1 in patients and testing this strategy in clinical trials.
If successful, targeting PRDX1 could open the door to combination therapies that make chemotherapy more effective, reduce toxic side effects, and improve treatment options for patients with some of the hardest-to-treat cancers.
Click here to read the full research paper in Oncotarget.
_______
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.