In this new study, researchers investigated an artificial intelligence (AI) tool that produces attenuation-corrected PET images while reducing radiation exposure for patients.
—
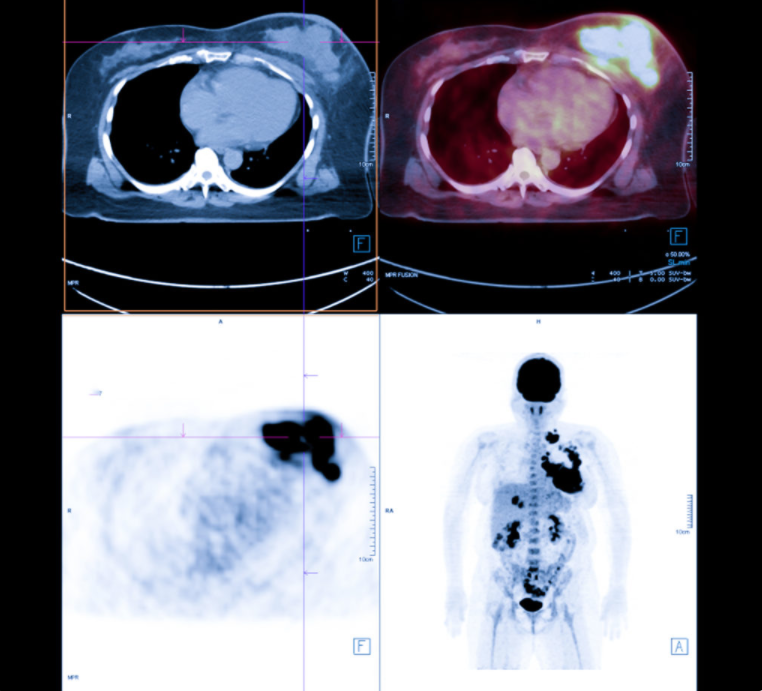
Positron Emission Tomography (PET) combined with Computed Tomography (CT) is a powerful imaging modality used in oncology for diagnosis, staging, and treatment monitoring. However, one limitation of PET/CT is the need for accurate attenuation correction (AC) to account for tissue density variations. Traditionally, low-dose CT scans are used for AC, but these contribute to patient radiation exposure.
In a new study, researchers Kevin C. Ma, Esther Mena, Liza Lindenberg, Nathan S. Lay, Phillip Eclarinal, Deborah E. Citrin, Peter A. Pinto, Bradford J. Wood, William L. Dahut, James L. Gulley, Ravi A. Madan, Peter L. Choyke, Ismail Baris Turkbey, and Stephanie A. Harmon from the National Cancer Institute proposed an artificial intelligence (AI) tool to generate attenuation-corrected PET (AC-PET) images directly from non-attenuation-corrected PET (NAC-PET) images, reducing the reliance on CT scans. Their research paper was published in Oncotarget’s Volume 15 on May 7, 2024, entitled, “Deep learning-based whole-body PSMA PET/CT attenuation correction utilizing Pix-2-Pix GAN.”
“Sequential PET/CT studies oncology patients can undergo during their treatment follow-up course is limited by radiation dosage. We propose an artificial intelligence (AI) tool to produce attenuation-corrected PET (AC-PET) images from non-attenuation-corrected PET (NAC-PET) images to reduce need for low-dose CT scans.”
The Study
The researchers developed a deep learning algorithm based on a 2D Pix-2-Pix generative adversarial network (GAN) architecture. They used paired AC-PET and NAC-PET images from 302 prostate cancer patients. The dataset was split into training, validation, and testing cohorts (183, 60, and 59 studies, respectively). Two normalization strategies were employed: Standard Uptake Value (SUV)-based and SUV-Nyul-based. The AI model learned to generate AC-PET images from NAC-PET images, effectively bypassing the need for CT scans during PET/CT studies. The performance of the AI model was evaluated at the scan level using several metrics:
- Normalized Mean Square Error (NMSE): A measure of the difference between predicted and ground truth AC-PET images. Lower NMSE indicates better performance.
- Mean Absolute Error (MAE): Similar to NMSE, lower MAE signifies improved accuracy.
- Structural Similarity Index (SSIM): Measures image similarity. Higher SSIM values indicate better alignment between AC-PET and ground truth images.
- Peak Signal-to-Noise Ratio (PSNR): Evaluates image quality. Higher PSNR values correspond to better image fidelity.
The AI model demonstrated promising results, achieving competitive performance across all metrics. The choice of normalization strategy (SUV-based or SUV-Nyul-based) did not significantly impact the model’s effectiveness.
The proposed AI tool has several clinical implications. By eliminating the need for low-dose CT scans, patients are exposed to less ionizing radiation during PET/CT studies. Additionally AC-PET images can be generated directly from NAC-PET data, simplifying the imaging process. The AI model also produces accurate AC-PET images, enhancing diagnostic confidence.
Conclusions
Deep learning-based AC-PET image generation using Pix-2-Pix GANs represents a promising approach to improve PET/CT imaging in prostate cancer patients. As AI continues to evolve, its integration into clinical practice may revolutionize how we acquire and interpret medical images, ultimately benefiting patient care. In summary, this research contributes to the ongoing efforts to enhance imaging techniques, reduce patient radiation exposure, and streamline clinical workflows.
“The Pix-2-Pix GAN model for generating AC-PET demonstrates SUV metrics that highly correlate with original images. AI-generated PET images show clinical potential for reducing the need for CT scans for attenuation correction while preserving quantitative markers and image quality.”
Click here to read the full research paper in Oncotarget.
—
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.