“Preclinical and clinical studies indicate that ferroptosis suppresses tumor growth, and dysregulation of ferroptosis promotes treatment resistance in cancer.”
Prostate cancer is one of the most common cancers in men. While treatment options have improved, advanced stages of the disease remain difficult to manage. One promising approach involves a process called ferroptosis. This is a type of programmed cell death that relies on iron and lipid oxidation to kill cancer cells by damaging specific fats in their outer membrane. These fats are especially vulnerable in environments with normal oxygen levels.
However, many prostate tumors grow in low-oxygen areas of the body, a condition known as hypoxia, where ferroptosis becomes less effective. A recent study, titled “Hypoxia induced lipid droplet accumulation promotes resistance to ferroptosis in prostate cancer,” and published on Oncotarget (Volume 16), explores how oxygen-poor environments help prostate cancer cells resist treatment and what strategies could help overcome this resistance.
The Study: How Low Oxygen Helps Prostate Cancer Resist Ferroptosis Treatments
A research team from the University of Arizona, led by Dr. Noel Warfel and Dr. Shailender Chauhan, studied how prostate cancer cells respond to ferroptosis-inducing drugs when oxygen levels are low. Their goal was to understand what changes happen inside cancer cells that help them survive under these conditions.
The Results: Prostate Cancer Cells Store Fats to Survive Ferroptosis in Low Oxygen Conditions
The researchers found that prostate cancer cells exposed to low-oxygen conditions were much less sensitive to ferroptosis-inducing drugs such as Erastin and RSL3. Even when the two drugs were combined to boost their effect, the cancer cells remained resistant.
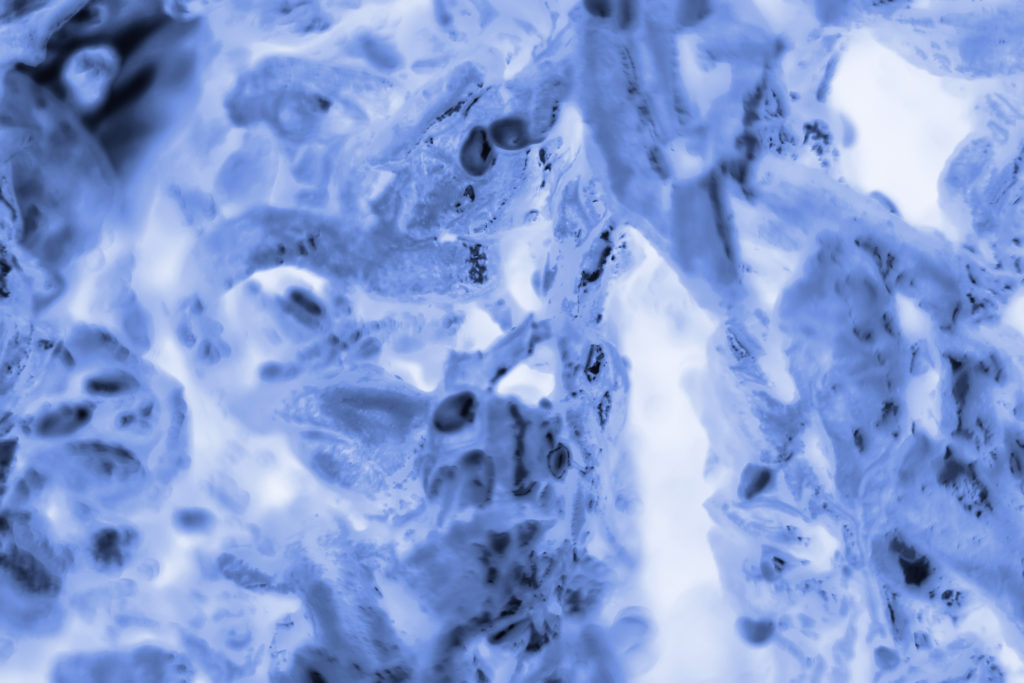
Under hypoxia, the cancer cells changed how they processed fats. They produced fewer of the fragile fats that are typically targeted by ferroptosis and instead created more stable fats, which were stored in small compartments called lipid droplets. These droplets acted like protective storage units, shielding the vulnerable fats from oxidative damage.
The study also showed that hypoxia reduced the activity of genes like ACSL4 and LPCAT3, which help incorporate polyunsaturated fatty acids into cell membranes, fats that are crucial for making cells susceptible to ferroptosis. At the same time, the levels of oxidation-prone fats like phosphatidylethanolamines decreased, while more stable lipids such as cholesteryl esters and triglycerides increased.
The researchers attempted to block lipid droplet formation, but the results varied depending on the cell type, suggesting that other factors may also contribute to this resistance.
The Impact: Targeting Fat Storage May Improve Prostate Cancer Treatment
This study highlights the critical role of the tumor microenvironment, especially oxygen levels, in shaping how cancer cells respond to treatment. It suggests that ferroptosis-inducing drugs alone may not be effective against tumors growing in low-oxygen conditions.
To overcome this resistance, future therapies could include inhibitors that block the enzymes or pathways responsible for lipid droplet formation, making cancer cells more vulnerable to ferroptosis.
Future Perspectives and Conclusion
This study provides valuable insight into how prostate tumors resist ferroptosis-based therapies and points to new treatment strategies. Targeting how cancer cells manage and store fats, by preventing the buildup of lipid droplets or releasing stored fats, may help restore their sensitivity to ferroptosis. While more research is needed to fully understand this mechanism, the findings mark a step toward more effective cancer treatments. This approach could also be applied to other solid tumors that show similar resistance in low-oxygen environments.
Click here to read the full research paper published by Oncotarget.
_______
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.