Researchers reveal their positive findings from a study of bacterial cancer therapy using a strain of Salmonella typhimurium in mouse-modeled prostate cancer.
The Trending with Impact series highlights Oncotarget publications attracting higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news and articles about the latest trending publications here, and at Oncotarget.com.
—
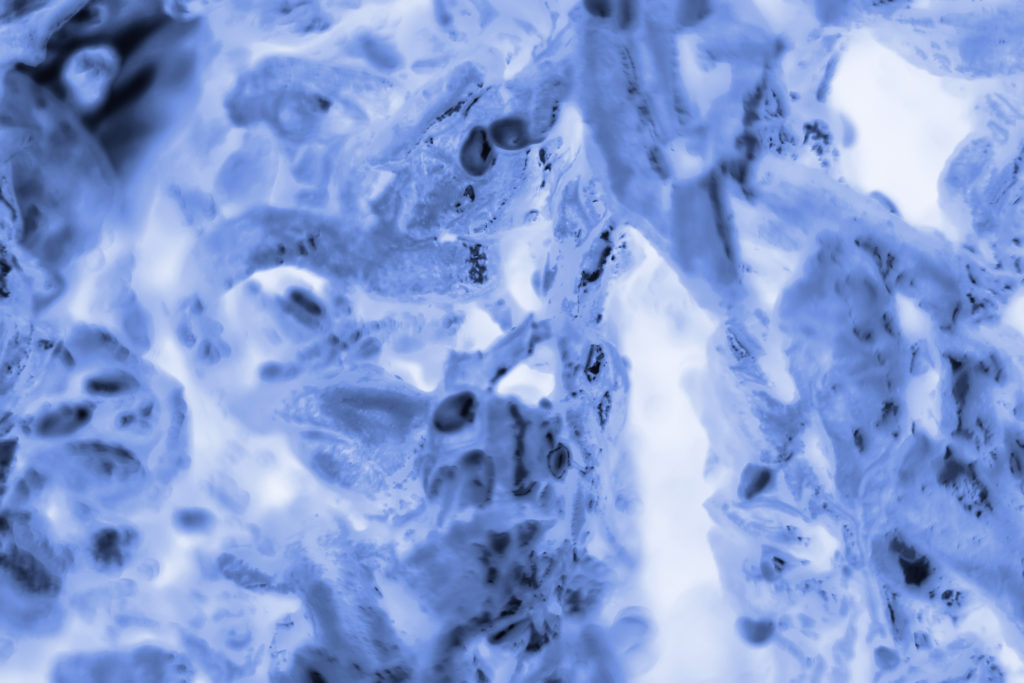
Over the past few decades, numerous studies have emerged using the promising strategy of bacteria as vehicles to deliver drugs or genes in tumor‐targeted therapies. Researchers say that bacterial cancer therapy may be able to overcome some of the limitations that conventional cancer therapy is stunted by, including the development of drug resistance.
Researchers in this study—from Yale University in Connecticut, the University of Missouri, the Harry S. Truman Memorial Veterans Hospital, and the Cancer Research Center in Missouri, and DeSales University in Pennsylvania, U.S.—used a Salmonella typhimurium strain (CRC2631) of bacteria (previously reported to have tumor-targeting capabilities) in prostate cancer-positive mouse-models and evaluated its toxicity, targeting ability, and genetic stability.
“Here, we report the toxicological and in vivo tumor-targeting profiles of CRC2631 in the syngeneic and autochthonous mouse model of aggressive prostate cancer, TRAMP (Transgenic Adenocarcinoma of Mouse Prostate).”
“The B6FVB TRAMP model recapitulates some of the key genetic aspects of human prostate cancer.”
The Study
“VNP20009 is considered as the safety benchmark in bacterial cancer therapy development because it has been safely administered in human cancer patients [7, 30].”
“To determine the safety profile of CRC2631, we performed CRC2631 and VNP20009 comparative toxicological studies in TRAMP animals.”
The team focused on measuring toxicity through treatment-related weight loss and lethality. Groups of 14-week-old B6FVB TRAMP-positive mice were scanned using magnetic resonance imaging. Four mice were dosed with CRC2631, and four were dosed with VNP20009; both treated four times per week. Mice were weighed and monitored daily for four weeks.
Since the CRC2631 bacteria are cleared out through the liver, the researchers also sought to establish the impact of CRC2631 on liver pathology in this bacterial cancer therapy. Two groups of 31-week-old B6FVB TRAMP-positive mice were observed, one treated with four doses of CRC2631 and the other with saline (the control group) at three-day intervals. They used histological staining in the liver to observe differences in necrosis, inflammation, and extramedullary hematopoiesis between CRC2631 and the control group. The team then tested for lethality and the maximum tolerated dose of CRC2631.
“Next, we sought to determine the in vivo tumor-targeting capability of CRC2631 in TRAMP animals.”
Using fluorescence imaging and a chloramphenicol resistance cassette, researchers were able to observe the biodistribution of CRC2631 to determine its tumor-targeting capability in TRAMP-positive mice. Since they knew that CRC2631 is filtered through the liver and that enriched colonies may be found here, researchers used the liver as a way to compare the bacterial load in tumor tissues.
The researchers also tested CRC2631’s genetic stability by gauging its likelihood of regaining toxicity and/or losing tumor targeting capability by performing longitudinal, whole genome sequencing and short nucleotide polymorphism analyses.
“To determine the genetic stability of CRC2631 inside the host, we performed longitudinal whole genome sequencing and short nucleotide polymorphism (SNP) analyses of CRC2631 prior to treatment and tumor-passaged CRC2631 in B6 TRAMP (+) mice.”
In vitro, CRC2631 directly kills prostate cancer cells, however, in vivo, it does not lead to decreased tumor burden. The researchers believe this may be due to the effects of some kind of resistance mechanism in vivo, and tested a combined treatment method of CRC2631 and Invivomab—a checkpoint blockade—in the mouse model.
“CRC2631 targets and directly kills murine and human prostate cancer cells in vitro (Supplementary Figure 2), raising the possibility that unknown resistance mechanisms protect tumor cells from CRC2631-mediated cell death in vivo.”
Results
Researchers explain that in the first two weeks of the study, mice treated with CRC2631 and VNP20009 lost a comparable amount of weight. However, in the second half of the study, VNP20009-treated animals lost progressively more weight than those treated with CRC2631. This revealed that CRC2631 is less toxic than VNP20009.
“Consistent with CRC2631 being less toxic than VNP20009, the median survival time was 142 days for VNP20009 compared to 186 days for CRC2631 (Figure 1F).”
After evaluating effects in the liver from CRC2631, they found no differences between CRC2631 and the control group in liver necrosis, inflammation, or extramedullary hematopoiesis.
“Thus, in contrast to VNP20009, CRC2631 does not cause overt liver pathology.”
They established the maximum tolerated dose to be two doses of 5 × 10^7 colony forming units, administered three days apart. In the model used in fluorescence imaging, they found that CRC2631 was significantly colonized in the tumor tissue of mice when compared to colonization in the liver and, as the dosage increased, CRC2631 quantities in tumor tissues also increased.
“Taken together, these data indicate that CRC2631^iRFP720-cat targets primary tumors and metastases.”
Researchers revealed that it would take approximately 9375 days for CRC2631 to acquire a potential mutation in any specific gene. They determined CRC2631 to be a genetically stable tumor-targeting mechanism. Next, they collected results from the CRC2631 and Invivomab immune checkpoint blockade combination.
“We turned our focus to an interaction between CRC2631 and immune cells and asked whether tumor-targeted CRC2631 generates an anti-tumor immune response that tumors rapidly inhibit via immune checkpoint mechanisms.”
They found that tumor burdens were significantly reduced in the combination treatment method, and ultimately, that CRC2631 treatment with a checkpoint blockade combination reduces the metastatic burden in mouse-modeled prostate cancer.
Conclusion
The study as a whole revealed to the researchers that CRC2631 safely targets primary tumors and metastases, is less toxic than VNP20009, does not cause overt liver pathology, and that, in combination with an immune checkpoint blockade such as Invivomab, it reduces metastatic burden in vivo in B6FVB TRAMP-positive mice.
“These findings indicate that CRC2631 is a genetically stable biologic that safely targets tumors. Moreover, tumor-targeted CRC2631 induces anti-tumor immune activity and concordantly reduces metastasis burden in the setting of checkpoint blockade.”
With more research, this method may soon be studied as an effective clinical treatment option for human prostate cancer.
Click here to read the full scientific study, published in Oncotarget.
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read—without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.
