“Latin America has been underrepresented in trials evaluating immunotherapy for hepatocellular carcinoma (HCC).”
Liver cancer, especially hepatocellular carcinoma (HCC), remains a major health concern worldwide. In Latin America, the situation becomes more difficult due to limited access to advanced treatments and the high prevalence of underlying liver diseases. A recent research paper, published in Volume 16 of Oncotarget by researchers from Argentina, Brazil, Chile, and Colombia, offers valuable insights into how patients in the region respond to a widely used immunotherapy regimen. This real-world study explores both the effectiveness of treatment and the risks of immune-related side effects.
Understanding Hepatocellular Carcinoma: Why It is So Difficult to Treat
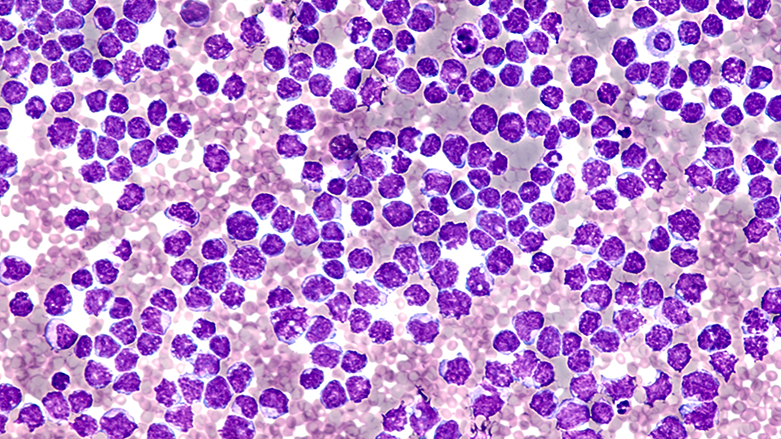
Hepatocellular carcinoma is often diagnosed at an advanced stage and frequently occurs in people with pre-existing liver conditions such as cirrhosis. Standard treatments like surgery or local therapies are not always possible in these cases. In recent years, the combination of two drugs—atezolizumab and bevacizumab—has shown promise in extending survival. However, most of the evidence comes from controlled clinical trials that may not represent the realities faced by healthcare providers and patients in Latin America.
The Study: Immunotherapy for Hepatocellular Carcinoma in Latin America
In a multicenter study titled “Immune-mediated adverse events following atezolizumab and bevacizumab in a multinational Latin American cohort of unresectable hepatocellular carcinoma,” led by Leonardo Gomes da Fonseca from Hospital das Clínicas, Universidade de São Paulo, Brazil, and Federico Piñero from Hospital Universitario Austral, Argentina, researchers aimed to fill that gap. The study included 99 patients with advanced HCC from Argentina, Brazil, Chile, and Colombia. All patients received the combination of atezolizumab and bevacizumab. The main objectives were to assess how frequently immune-related side effects, known as immune-related adverse events (irAEs), occurred and whether these events affected overall survival.
The Results: Immune-Related Adverse Events
Immunotherapy works by boosting the immune system to fight cancer. However, this can also lead to unintended effects where the immune system attacks healthy tissues. These irAEs can range from mild symptoms to serious conditions like liver inflammation, which can be particularly dangerous for patients whose liver function is already damaged.
In this study, the median overall survival was 17 months, a result consistent with international clinical trials. About 18% of patients developed irAEs, most commonly hepatitis, thyroiditis, and nephritis. Nearly half of these cases required medical treatment such as corticosteroids. Even so, only about half of the irAEs were completely resolved. Importantly, the occurrence of irAEs did not appear to reduce overall survival, suggesting that while these side effects require attention, they are manageable.
An additional finding was that patients with higher levels of alpha-fetoprotein (AFP), a marker often used to assess liver cancer severity, were more likely to develop irAEs. This could help clinicians identify which patients need closer monitoring during treatment.
Implications for Hepatocellular Carcinoma Care in Latin America
This is one of the few studies assessing how HCC patients in Latin America respond to immunotherapy in everyday clinical settings. The results support the use of atezolizumab and bevacizumab in the region but also point out the importance of being prepared to detect and manage side effects. Building medical capacity for early identification and treatment of irAEs is especially important for patients with weaker liver function.
Future Perspectives and Conclusion
Although immune-related side effects did not seem to affect survival in this study, they add another layer of complexity to HCC treatment. More research is needed to understand which patients are most at risk and how to prevent these side effects. For the moment, this study provides useful information for clinicians and healthcare systems aiming to safely expand access to immunotherapy in Latin America for HCC.
Click here to read the full research paper in Oncotarget.
_______
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com.
Oncotarget is indexed and archived by PubMed/Medline, PubMed Central, Scopus, EMBASE, META (Chan Zuckerberg Initiative) (2018-2022), and Dimensions (Digital Science).
Click here to subscribe to Oncotarget publication updates.
For media inquiries, please contact media@impactjournals.com.