Researchers investigated the efficacy of HDAC inhibitors in combination with PARP inhibitors and chemotherapeutic drugs in multiple blood cancer cell lines.
Chromatin constitutes chromosomes in eukaryotic cells and comprises DNA and proteins. Chromosomes produce proteins and enzymes that are essential for cellular function and maintenance, including DNA repair. A critical process for DNA repair is poly(ADP-ribosyl)ation, or PARylation.
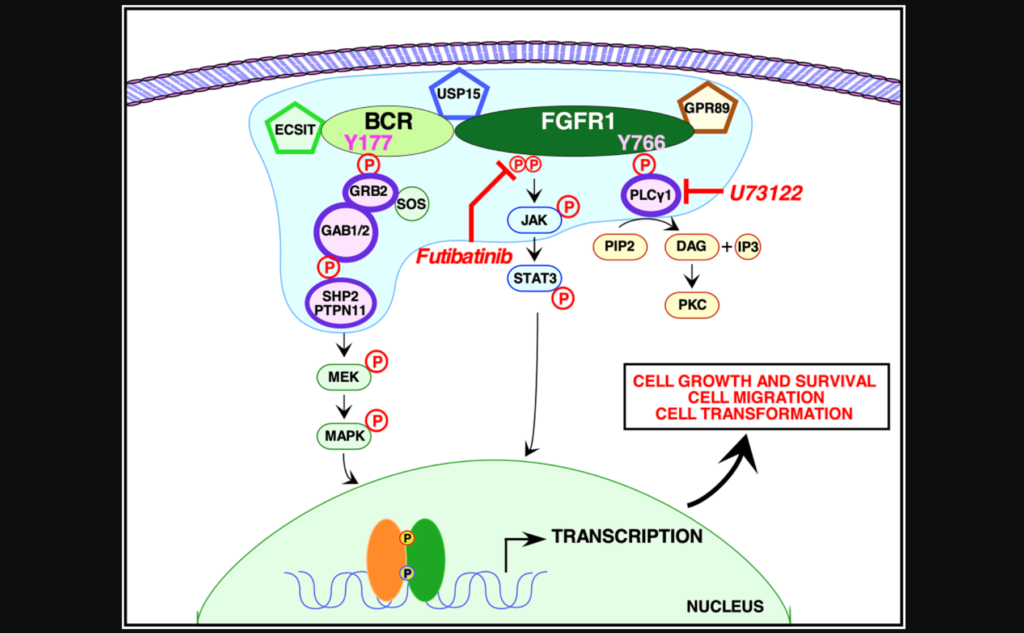
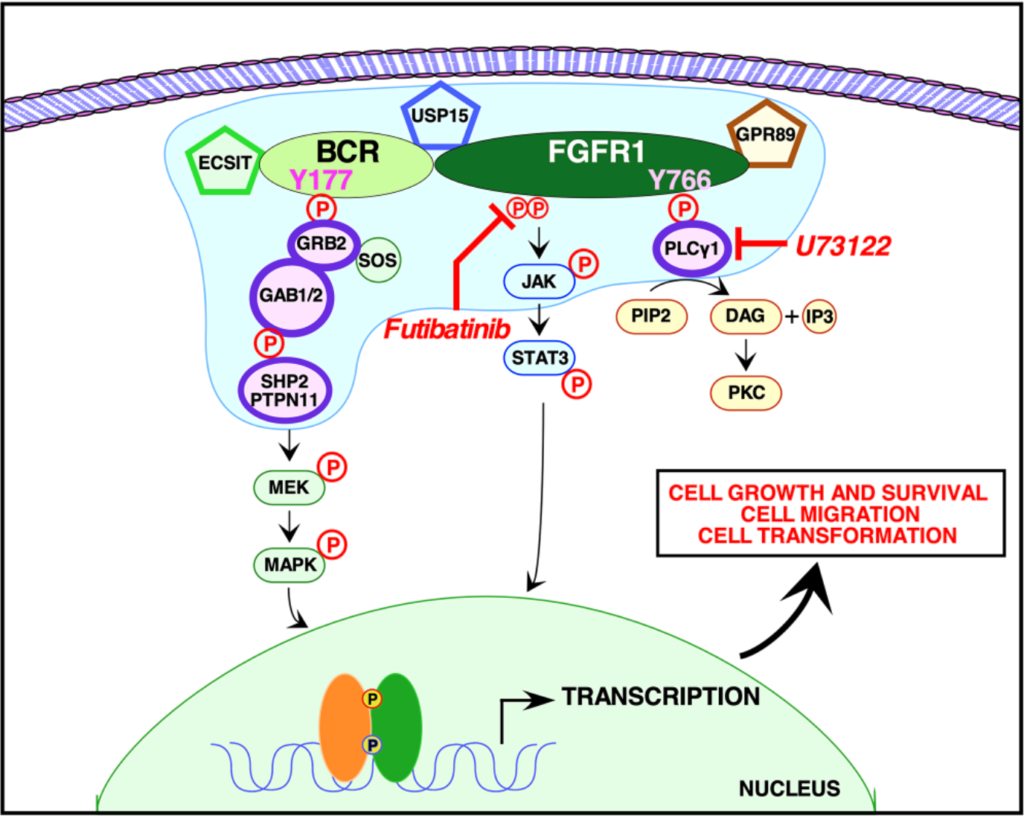
PARylation is triggered by poly(ADP ribose) polymerase (PARP) enzymes. When DNA becomes damaged, PARP enzymes bind to the damaged location in the cell. In cancer cells, however, this natural process can be counterproductive in respect to cancer treatment. PARylation can produce DNA repair mechanisms in cancer cells that can lead to cell death evasion and even drug resistance. Inhibiting PARylation may be a viable therapeutic strategy for cancer treatment.
HDAC Inhibitors
Histones, the main proteins that constitute chromatin, undergo post-translational modifications that regulate gene expression. Histone acetylation is an important epigenetic process that affects gene expression by relaxing the chromatin structure, making chromatin remodeling more feasible. Histone deacetylases (HDACs) are enzymes that can have the opposite effect. Histone deacetylation makes the chromatin more compact and difficult to remodel. The overexpression of HDAC has also been associated with tumorigenesis. Histone deacetylase inhibitors (HDACi) are a class of therapeutics that have shown promise in the treatment of hematologic malignancies (blood cancer) and solid tumors.
“Overexpression of HDACs has been associated with tumorigenesis by down-regulation of tumor suppressor genes [3, 4]; hence, HDAC inhibitors (HDACi) including vorinostat (SAHA), romidepsin (Rom), panobinostat (Pano) and belinostat have been approved by the United States Food and Drug Administration for the treatment of hematologic and other malignancies [5]. These inhibitors restore appropriate gene expression, resulting in induction of cell differentiation, cell cycle arrest and apoptosis [6].”
The Study
In a new study, researchers Benigno C. Valdez, Yago Nieto, Bin Yuan, David Murray, and Borje S. Andersson from the Department of Stem Cell Transplantation and Cellular Therapy at the University of Texas MD Anderson Cancer Center and the Cross Cancer Institute’s Department of Experimental Oncology at the University of Alberta investigate the efficacy of HDACi in combination with PARP inhibitors (PARPi) and chemotherapeutic drugs to treat hematologic cancer. On October 14, 2022, their research paper was published in Volume 13 of Oncotarget, entitled, “HDAC inhibitors suppress protein poly(ADP-ribosyl)ation and DNA repair protein levels and phosphorylation status in hematologic cancer cells: implications for their use in combination with PARP inhibitors and chemotherapeutic drugs.”
“Despite their preclinical efficacy, HDACi do not seem to be clinically highly effective as monotherapy, and potentially more effective anti-tumor activity is observed when they are combined with other anti-cancer drugs [7–9].”
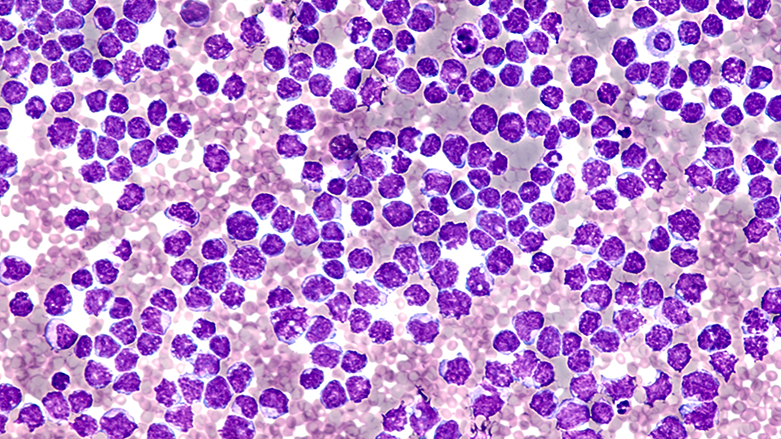
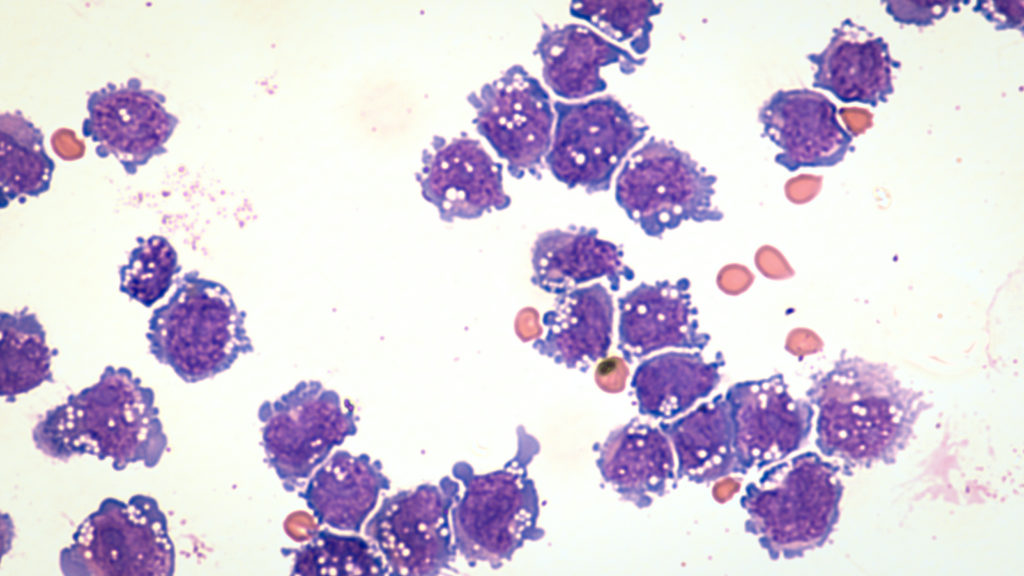
Studies on the interactions of HDACi with PARPi in cancers of the blood are limited, especially when combined with chemotherapeutic agents. The researchers used a panel of hematologic cancer cell lines (acute myeloid leukemia, T-cell acute lymphoblastic leukemia, chronic myeloid leukemia, and multiple myeloma) and patient-derived cell samples to study the effect of HDACi (including SAHA (Vorinostat), panobinostat (Pano), romidepsin (Rom) and trichostatin A (TSA)) on PARylation. In addition, the team looked at the efficacy of HDACi combined with PARPi, including Olaparib (Ola) and niraparib (Npb), and with chemotherapeutic agents gemcitabine (Gem), busulfan (Bu) and melphalan (Mel).
Results
The researchers found that hematologic cancer cell lines and patient-derived cell samples exposed to various HDACi resulted in a significant caspase-independent inhibition of protein PARylation. HDACi-mediated inhibition of protein PARylation was mainly catalyzed by PARP1. These findings suggest that HDACi could potentially be used in combination with PARP inhibitors and chemotherapeutic drugs to treat blood cancers.
“Our results indicate that the anti-tumor efficacy of HDACi is partly due to down-regulation of PARylation, which negatively affects the status of DNA repair proteins. This repair inhibition, combined with the high levels of oxidative and DNA replication stress characteristic of cancer cells, could have conferred these hematologic cancer cells not only with a high sensitivity to HDACi but also with a heightened dependence on PARP and therefore with extreme sensitivity to combined HDACi/PARPi treatment and, by extension, to their combination with conventional DNA-damaging chemotherapeutic agents. The observed synergism of these drugs could have a major significance in improving treatment of these cancers.”
Conclusion
HDACi drugs can inhibit PARylation. The combination of HDACi-mediated inhibition of PARylation was complemented by PARPi and chemotherapeutic agents in multiple blood cancer cell lines. The efficacy of this combined treatment was superior to that of any single agent, supporting the further clinical development of HDACi in cancer therapy. These findings could potentially be used to improve the treatment of hematologic cancers.
“In conclusion, our results provide a molecular explanation for the HDACi-mediated inhibition of DNA repair in hematologic cancer cells and support the combinatorial application of HDACi, PARPi and chemotherapeutic agents for the treatment of hematologic malignancies.”
Click here to read the full research paper published by Oncotarget.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is an open-access journal that publishes primarily oncology-focused research papers in a continuous publishing format. These papers are available at no cost to readers on Oncotarget.com. Open-access journals have the power to benefit humanity from the inside out by rapidly disseminating information that may be freely shared with researchers, colleagues, family, and friends around the world.
For media inquiries, please contact media@impactjournals.com.