Two gene variants were studied in large-scale cohorts for their potential roles in bladder and kidney cancer among Polish patients.

Genitourinary cancers are a group of cancers that affect components of the urinary tract, including the bladder and kidneys. Worldwide, bladder and kidney cancer impact men at disproportionately higher rates than women. While incidence and mortality rates of bladder cancer in most western European countries have been consistently decreasing, some countries in the region, such as Poland, have seen an increase. Bladder cancer is the 4th most common malignancy in Polish men and the 14th most common malignancy in Polish women. There is currently a need to identify more effective bladder cancer biomarkers and therapeutic targets to develop new effective treatments that improve patient outcomes.
“The association between the NOD2 c.3020insC allele and CDKN2A missense variant c.442G>A (p.P.A148T) and survival of patients with bladder or kidney cancer remains controversial.”
In April of 2022, researchers from Pomeranian Medical University, University of Newcastle and NSW Health Pathology published the first larger-scale study in Poland to describe the clinical characteristics and survival of bladder cancer patients and kidney cancer patients associated with variants in NOD2 and CDKN2A. Their research paper was published in Oncotarget on April 22, 2022, and entitled, “Bladder cancer survival in patients with NOD2 or CDKN2A variants.”
The Study
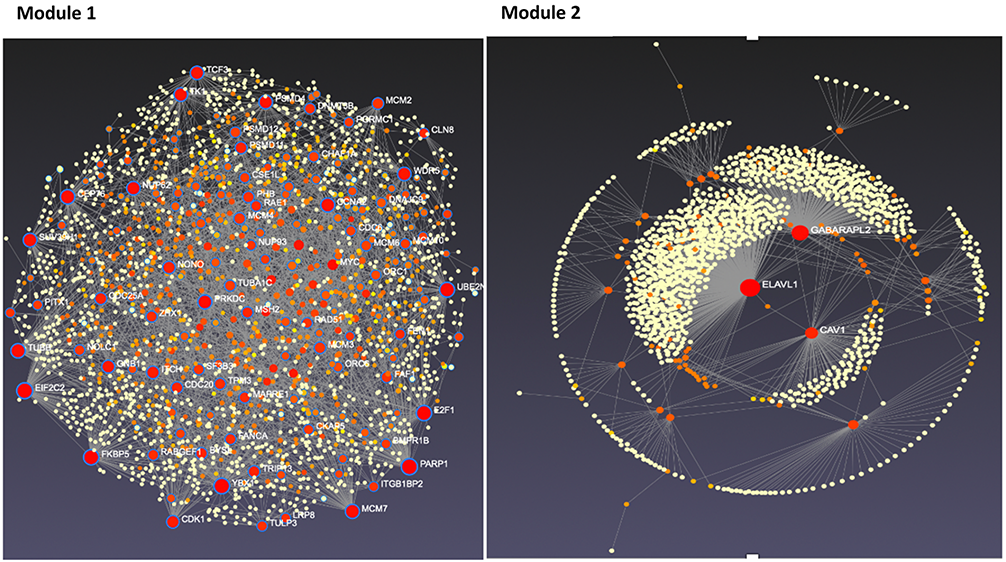
In this study, the researchers investigated two gene variants—the NOD2 c.3020insC variant and the CDKN2A p.A148T polymorphism—and their role in bladder and kidney cancer in Polish cohorts. This NOD2 variant has been shown to occur in 7.3% of the Polish population. The CDKN2A polymorphism has been found in 3.5% of the Polish population. Therefore, these gene variants could be considered genetic risk factors for cancer. To test this hypothesis, the researchers assembled detailed participant data from a cohort of 706 bladder cancer patients and 410 kidney cancer patients. The team compiled control data from over 5,000 unselected, cancer-free individuals.
“To our knowledge, this is the first larger-scale study describing the clinical characteristics and survival of bladder and kidney cancer patients that is associated with the NOD2 c.3020insC allele and the CDKN2A p.A148T polymorphism in Poland.”
After performing the variant analysis in the cohort of Polish patients with bladder cancer, the team found that 8.9% of these patients carried the NOD2 variant and 5.2% carried the CDKN2A variant. However, their analysis revealed that neither the NOD2 nor the CDKN2A variant played a significant role in the survival of patients with bladder cancer. In performing the variant analysis in the cohort of Polish patients with kidney cancer, they found that 7.3% of these patients carried the NOD2 variant and 3.4% carried the CDKN2A variant. The researchers did not observe any statistically significant relationship between kidney cancer and either variant. However, they were not able to perform a survival analysis in the kidney cancer cohort.
Conclusion
The researchers found that the NOD2 c.3020insC variant and the CDKN2A p.A148T polymorphism were not significantly associated with the survival of bladder cancer patients, regardless of age, cancer family history, smoking status, and sex. To date, this is the first larger-scale study to examine these variants in association with clinical characteristics and survival of Polish patients with bladder cancer.
“In summary, the results of this study indicate that neither the NOD2 c.3020insC variant or the CDKN2A p.A148T polymorphism are associated with the survival of bladder cancer patients regardless of age, cancer family history, smoking status, and sex. Thus, the NOD2 c.3020insC or the CDKN2A p.A148T polymorphism cannot be added to the list of genes that are associated with an increased susceptibility to bladder or kidney cancer at this time.”
Click here to read the full research paper published by Oncotarget.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is an open-access journal that publishes primarily oncology-focused research papers in a continuous publishing format. These papers are available at no cost to readers on Oncotarget.com. Open-access journals have the power to benefit humanity from the inside out by rapidly disseminating information that may be freely shared with researchers, colleagues, family, and friends around the world.
For media inquiries, please contact media@impactjournals.com.